New Possibilities of Using Aerolase Nd:YAG 1064nm and Er:YAG 2940nm Microsecond Lasers in Facial Rejuvenation
N.N. Geraskova1, S.I. Surkichin, M.D.2 , N.V. Gryazeva, M.D.3 , E.K. Teplova1
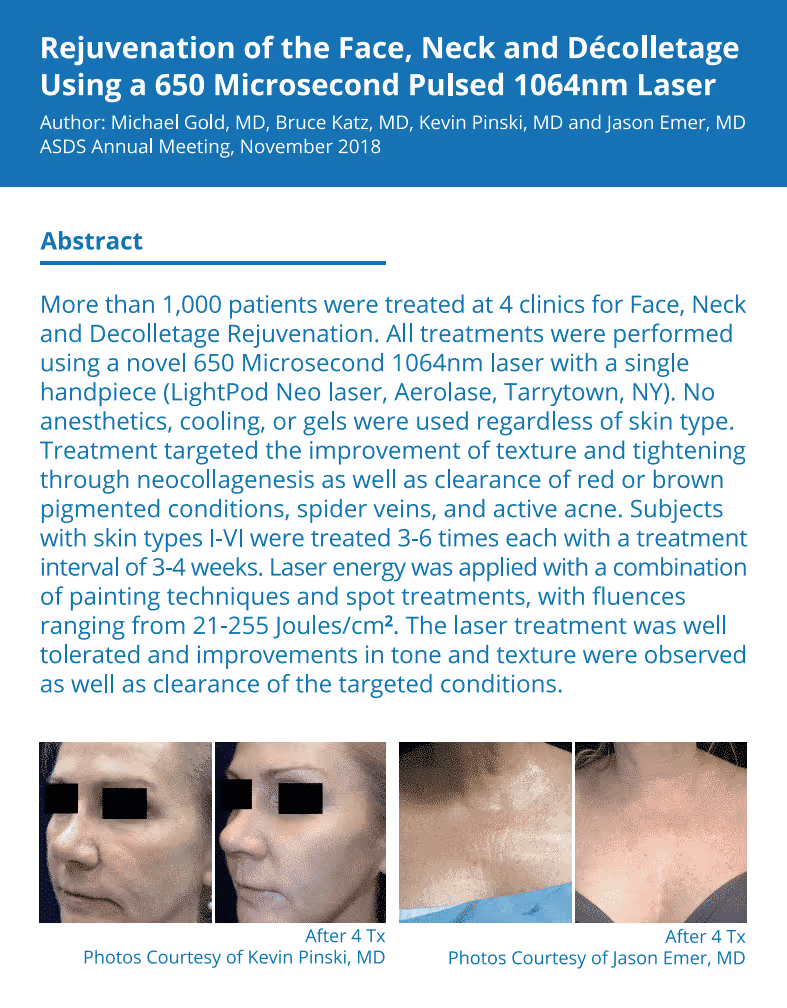
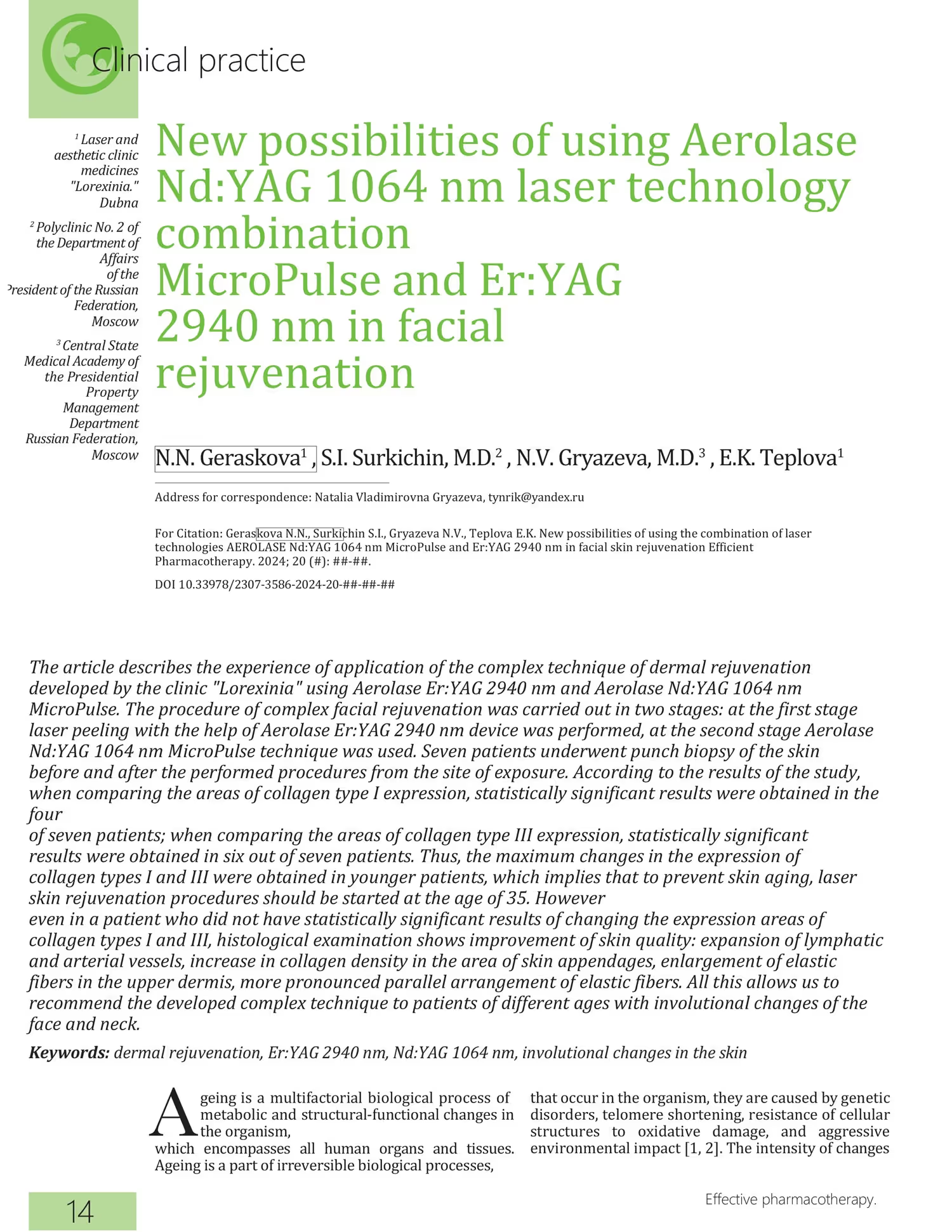
The article describes the experience of application of the complex technique of dermal rejuvenation developed by the clinic "Lorexinia" using Aerolase Er:YAG 2940 nm and Aerolase Nd:YAG 1064 nm MicroPulse. The procedure of complex facial rejuvenation was carried out in two stages: at the first stage laser peeling with the help of Aerolase Er:YAG 2940 nm device was performed, at the second stage Aerolase Nd:YAG 1064 nm MicroPulse technique was used. Seven patients underwent punch biopsy of the skin before and after the performed procedures from the site of exposure. According to the results of the study, when comparing the areas of collagen type I expression, statistically significant results were obtained in the four of seven patients; when comparing the areas of collagen type III expression, statistically significant results were obtained in six out of seven patients. Thus, the maximum changes in the expression of collagen types I and III were obtained in younger patients, which implies that to prevent skin aging, laser skin rejuvenation procedures should be started at the age of 35. However even in a patient who did not have statistically significant results of changing the expression areas of collagen types I and III, histological examination shows improvement of skin quality: expansion of lymphatic and arterial vessels, increase in collagen density in the area of skin appendages, enlargement of elastic fibers in the upper dermis, more pronounced parallel arrangement of elastic fibers. All this allows us to recommend the developed complex technique to patients of different ages with involutional changes of the face and neck.
Keywords: dermal rejuvenation, Er:YAG 2940 nm, Nd:YAG 1064 nm, involutional skin changes.
Introduction
Aging is a multifactorial biological process of metabolic and structural-functional changes in the organism, which encompasses all human organs and tissues. Aging is a part of irreversible biological processes that occur in the organism, they are caused by genetic disorders, telomere shortening, resistance of cellular structures to oxidative damage, and aggressive environmental impact [1, 2]. The intensity of changes is influenced by a group of factors that are not directly related to age: endocrine disorders, psychological traumas, overdose of ultraviolet and X-ray radiation, significant fluctuations in body weight, unfavorable ecology, harmful working conditions, and a number of other factors [2]. As a result of these factors, various histomorphological and physiological mechanisms are formed, which influence the nature, degree, and speed of development of changes in various skin structures. Properties and functions of the skin and its appendages deteriorate with age: the skin loses moisture, ability to regenerate, thins, the processes of keratinization, pigmentation, moisture retention, blood circulation, collagen synthesis, etc. are disturbed. [3].
A wide range of methods of treatment at the modern stage of cosmetology and physiotherapy methods allows you to choose individual programs taking into account the specifics of the skin and budget.
So-called dermal skin rejuvenation is becoming increasingly popular nowadays. This term means restructuring of the dermis with a sharp increase in the amount of collagen types I and III and changes in tissue perfusion due to normalization of the microcirculatory system. Various lasers are usually used to achieve these effects.
Lasers commonly used for rejuvenation can be divided into ablative and non-ablative lasers, both of which can be fractionated [4]. Traditionally, ablative lasers such as carbon dioxide (CO2 , 10,600 nm) or erbium (Er:YAG, 2490 nm) lasers are considered more effective than non-ablative devices [5, 6]. However, after the laser procedure, it takes a long time for the skin to recover and there is a high probability of complications [7]. To minimize these complications, fractionation technology has been introduced [8]. Er:YAG lasers remove excess tissue without causing significant lateral thermal heating [5]. Compared to fractionated CO2 , the fractionated Er:YAG laser provides similar efficacy with a more satisfactory safety profile [6]. At the same time, non-ablative devices are used for skin rejuvenation [7-10]. For example, a short-pulse neodymium laser on yttrium-aluminum garnet (Nd:YAG) with a wavelength of 1064 nm can deliver energy to the deep layers of the dermis, which leads to collagen and elastin remodeling with minimal or no rehabilitation period and with less discomfort for the patient [7]. In addition, Nd:YAG laser pulses are poorly absorbed by melanin, which allows for safer laser treatment in patients with any skin phototype [8]. Thus, the combined use of Er:YAG- and Nd:YAG-lasers is the most preferable to achieve the maximum effect of skin restructuring.
In order to study the effectiveness of combined application of Er:YAG- and Nd:YAG-laser on the basis of the Lorexinia Clinic and Polyclinic No. 2 of the Russian Presidential Administration, a study was conducted with the participation of 25 female volunteers with involutional changes in the skin of the face and neck aged 38 to 61 years. The average age was 49 ± 3.7 years. All patients underwent a complex procedure using Aerolase Er:YAG 2940 nm and Aerolase Nd:YAG 1064 nm MicroPulse. Seven patients underwent panch biopsy of the skin before and after the procedures from the treatment site.
The procedure of complex facial rejuvenation was carried out in two stages: the first stage was laser peeling using the AEROLASE Er:YAG 2940 nm device. The treatment was performed with a defocused laser beam with a wavelength of 2940 nm, pulse duration of 0.3 ms, pulse energy of 0.6 J, spot area up to 1 cm2 , which contributed to the reduction of energy density below the threshold values for ablation. This, in its turn, made it possible to achieve, while preserving photobiological effects in the form of skin tightening and thickening, improvement of its photo-optical properties, instead of ablation, a soft change of superficial skin layers in the form of large-plate peeling with improvement of its relief. Also due to subcoagulation laser heating of the skin there was an activation of heat shock proteins leading to the launch of neocollagenogenesis process. At the second stage we used the Aerolase Nd:YAG 1064 nm MicroPulse technique, which allowed us to achieve the following two effects:
- Small-point coagulation of dermal vessels and coagulation-denaturation changes in the dermis (destruction of "old" collagen) were achieved with the laser beam with a wavelength of 1064 nm, pulse duration of 0.65 ms, pulse energy of 3 J, and spot diameter of 0.2 cm. Since the main chromophore for 1064 nm radiation is hemoglobin, the factor of microcirculatory channel destruction triggers neoangiogenesis, significantly changing the total tissue perfusion, which is an additional rejuvenation factor.
- Further, with increasing the pulse energy up to 6 J and spot diameter up to 0.5 cm, subcoagulative laser heating of the skin was achieved, which stimulated tissue response to heat shock, which is manifested by a temporary change in cell metabolism. The heat shock proteins formed as a result of laser treatment trigger local immunity reactions in the form of aseptic inflammation. The result of the procedure is the start of the neocollagenogenesis process with predominant synthesis of collagen types I and III with an obvious increase in the amount of collagen type I. The clinical result is an increase in the density and thickness of the dermis and restoration of the mechanical properties of the skin.
In order to objectify the results of the study before and one month after the procedure, biopsy specimens were taken from the temporal, cervical, and parotid regions. For histological examination, 4-6 µm thick sections were prepared and stained with hematoxylin (HE) and eosin according to the Van Gieson method (V-G). For immunohistochemical (IHC) staining, serial slices 4-6 µm thick were made and placed on slides coated with poly-L-lysine (Menzel). Studies were performed on deparaffinized and dehydrated sections using the avidin-biotin immunoperoxidase method. Primary antibodies were used to verify expression.
The obtained micro specimens were scanned using a Leica Aperio AT2 preparations scanner and subsequently analyzed using Aperio ImageScope software.
The relative area of expression was determined for marker studies. At least five fields of view were analyzed at a magnification of ×40 and the relative expression area was measured. The relative expression area was calculated as the ratio of the marker expression area to the area of the tissue under study.
Clinical Cases
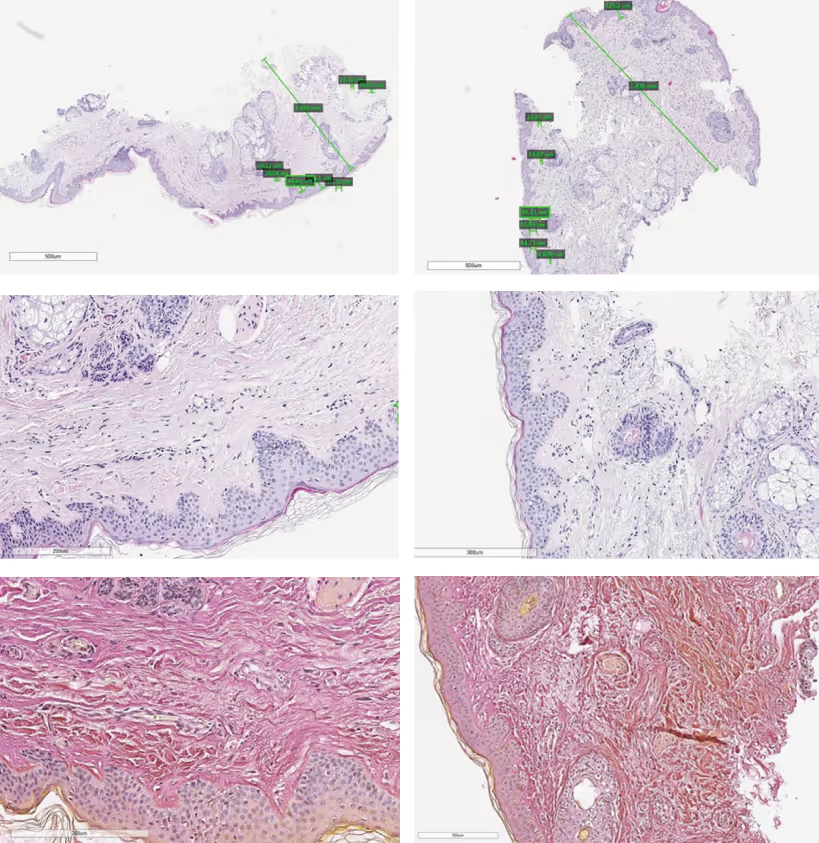
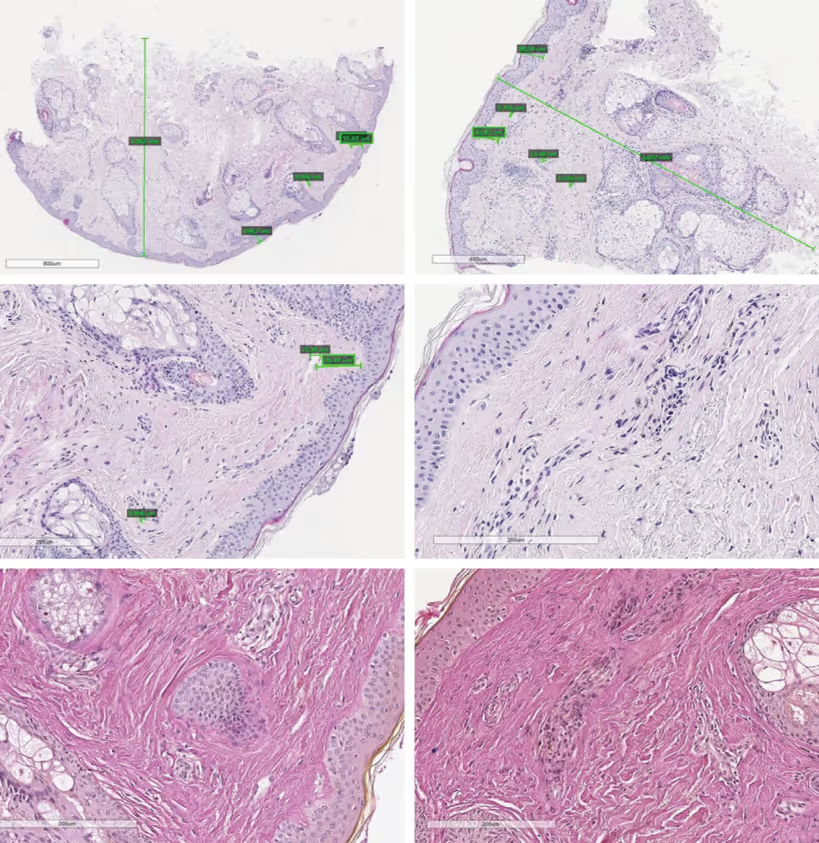
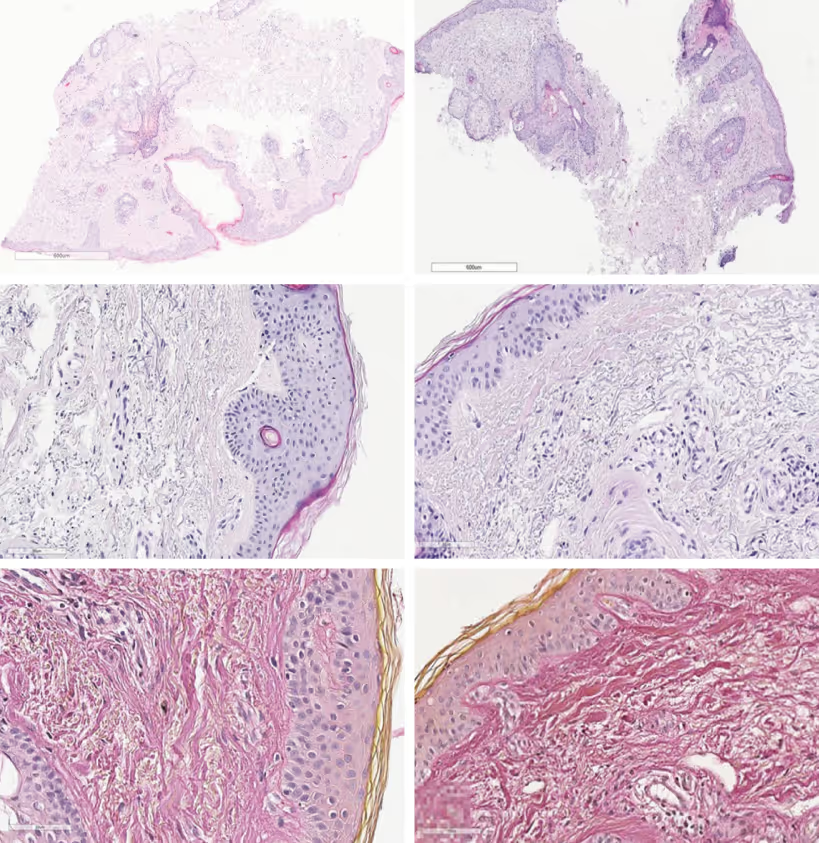
Patient K., 42 years old. Before treatment, the histologic preparation showed epidermis with foci of hyperkeratosis and acanthosis, foci with the formation of horny cysts. The papillary dermis consisted of loose, thin collagen with foci of thickening in the zone of skin appendages. Spasmodic vessels, single dilated arterioles with weak lymphocytic infiltration, single lymphatic capillaries and loose pigment, as well as abundance of sebaceous glands were visualized. The dermis is represented by loose, thin connective tissue fibers (pink) and few elastic fibers (yellow) (Fig. 1).
After therapy, the histologic picture changed: a small number of melanocytes in the epidermis and loose pigment in the dermis, as well as dilation of lymphatic vessels and minimal changes in the arterial channel were observed. A moderate lymphocytic infiltrate was detected perivasally. In B-G staining, the dermis was represented by loose collagen with an increase in density in the appendages zone, elastic fibers were visible in a small amount. In the upper dermis, the fibers had enlarged, acquiring a more pronounced parallel arrangement.
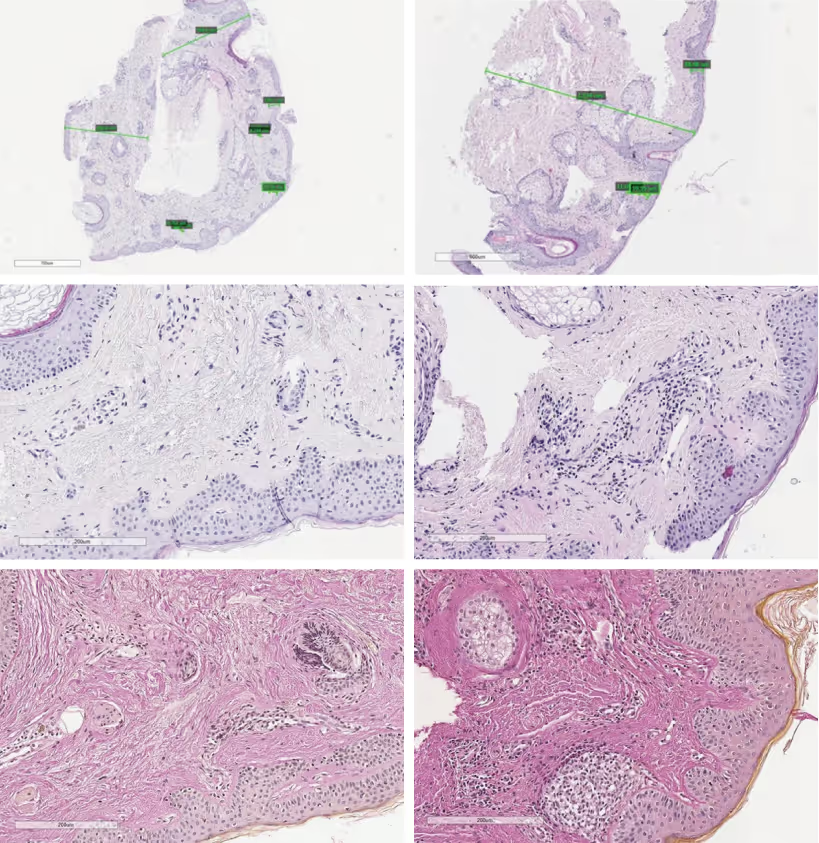
The results of the samples comparison showed a weak perivasal inflammatory reaction and collagen thickening in the dermis with more parallel orientation of the bundles (Fig. 2).
The mean expression area of type I collagen was 59.52 before treatment and 54.19 after; type III collagen was 5.83 before treatment and 7.65 after. When comparing no statistically significant difference was found in the expression areas of collagen types I and III before and after exposure (p > 0.05).
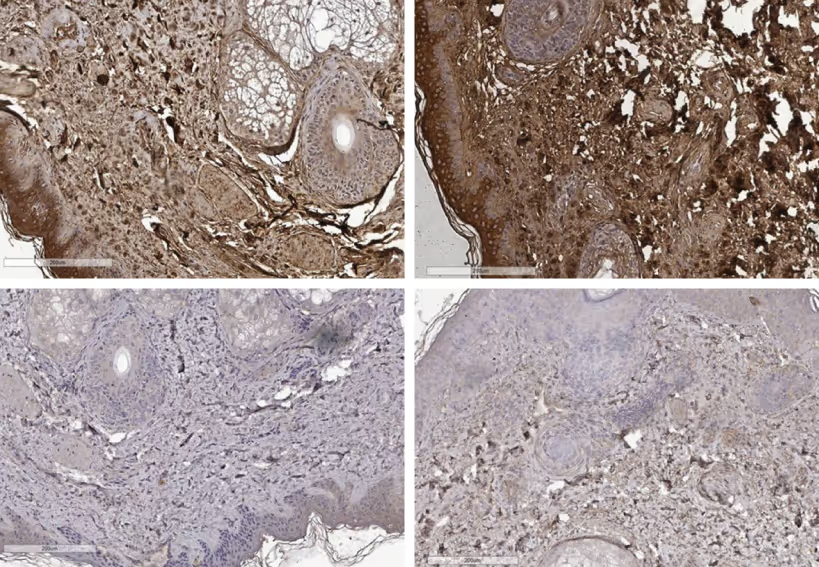
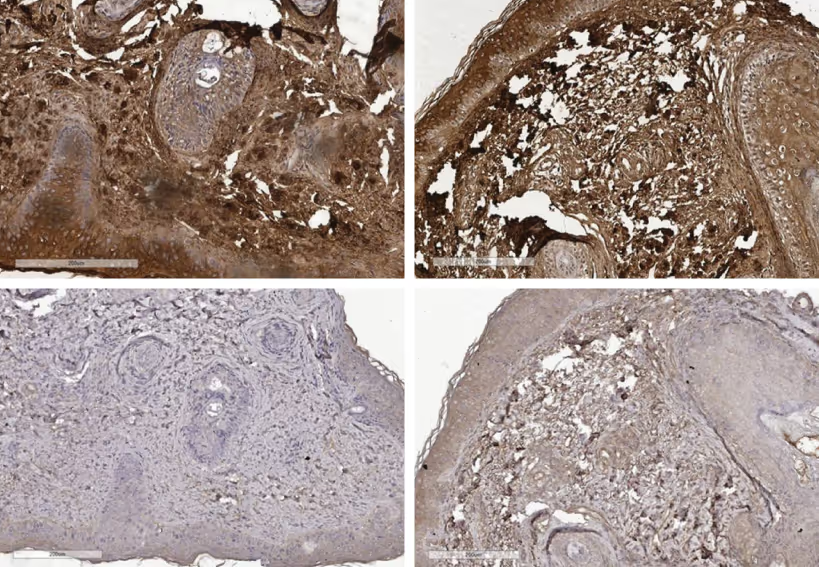
Patient S., 61 years old. The patient was diagnosed with a combined skin type, oily in the T-zone, photo-type II, even relief, pronounced hyperkeratosis. Before treatment the histologic preparation showed epidermis with hyperkeratosis, foci of acanthosis, single melanocytes with pigment. The middle dermis contained foci of dense collagen with fragmentation; hair follicles; hair raising muscle and sebaceous glands of typical structure; sweat glands with lipomatosis; vessels represented by full blood arteries and lymphatic capillaries. In B-G staining, the upper dermis has dense mature collagen (red) with fragmentation. The middle dermis is represented by loose, thin and medium connective tissue fibers (pink) and single elastic fibers (yellow).
After therapy, B-G staining showed loose thin collagen and disintegration in the upper dermis; smooth muscle proliferation was detected in the deep layers; elastic fibers were found in small amounts (Fig. 3).
When comparing the samples, more pronounced rough collagenization and small changes in the vascular channel in the form of lumen widening were noted (Fig. 4). The average expression area of collagen type I before treatment was 49.43, after - 75.8, collagen type III before treatment - 1.24, after - 5.08. When comparing the expression areas of collagen types I and III before and after treatment, a statistically significant difference was revealed (p < 0.05).
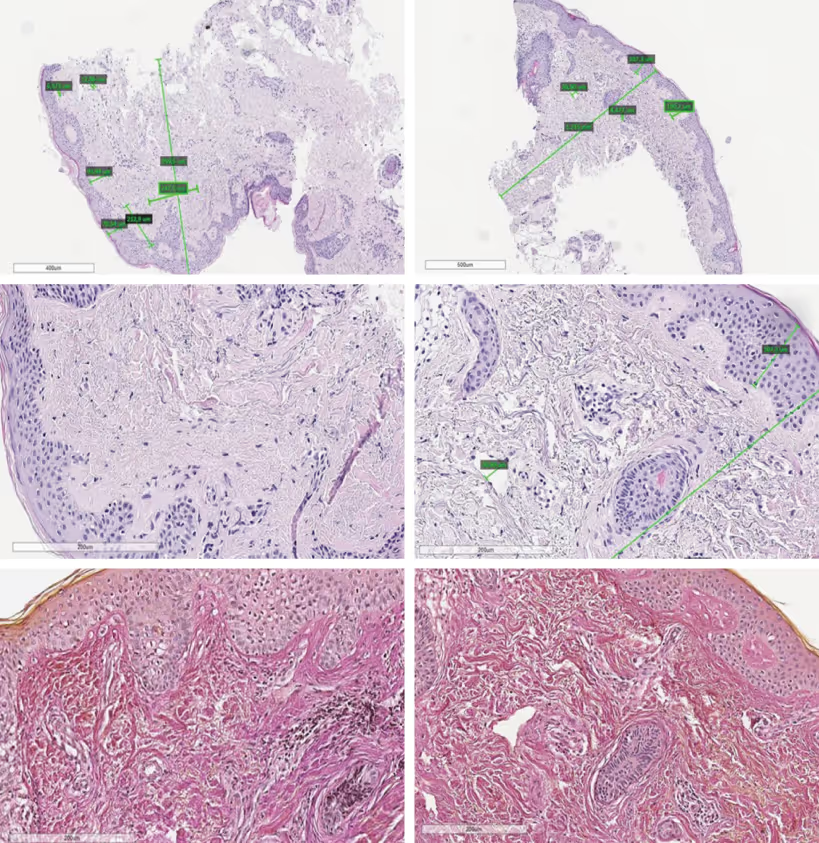
Patient V., 38 years old. The patient has normal skin type, II phototype, smooth relief, follicular hyperkeratosis in the T-zone.
Before treatment, the histologic preparation showed epidermis of typical structure. The middle dermis was loose, containing hair follicles, hair-lifting muscle, sebaceous and sweat glands. The subcutaneous and upper dermis was represented by loose connective tissue with a small number of vessels; the lumen was rounded; single lymphatic capillaries with a narrow lumen. In B-G staining, the dermis was represented by loose, thin and medium connective tissue fibers (pink) and numerous elastic fibers (yellow).
After laser exposure, the dermis was also represented by loose, thin and medium fibers of connective tissue (pink) and few elastic fibers (yellow), the course of fibers was chaotic (Fig. 5). No significant differences were found when comparing the samples among themselves (Fig. 6).
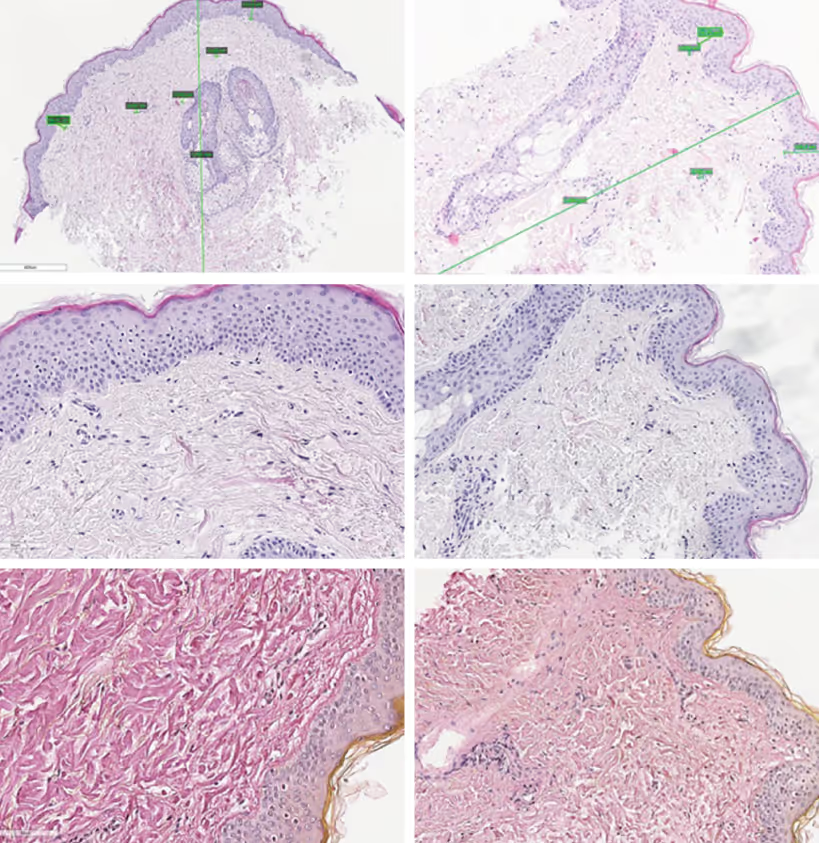
The average expression area of collagen type I before treatment was 65.67, after 82.40, collagen type III before treatment - 3.10, after - 2.08. When comparing the expression areas of collagen types I and III before and after laser treatment, a statistically significant difference was revealed (p < 0.05).
Patient T., 39 years old. The patient has a normal skin type, phototype II, smooth relief. Before treatment, the histologic preparation showed epidermis of typical structure. The upper dermis was loose, the middle dermis contained hair follicles; hair raising muscle; abundance of sebaceous glands. The surrounding dermis was represented by dense, large bundles of connective tissue; single lymphatic capillaries with a wide lumen; the lumen of vessels was narrow. In B-G staining before and after therapy, the dermis was represented by thick, large connective tissue fibers; elastic fibers were detected in small amount (Fig. 7).
When comparing the samples with each other, insignificant changes of lymphatic vessels with their dilation and appearance of lymphocytic infiltration with thickening of the infiltrate in the area of omental glands are determined (Fig. 8).
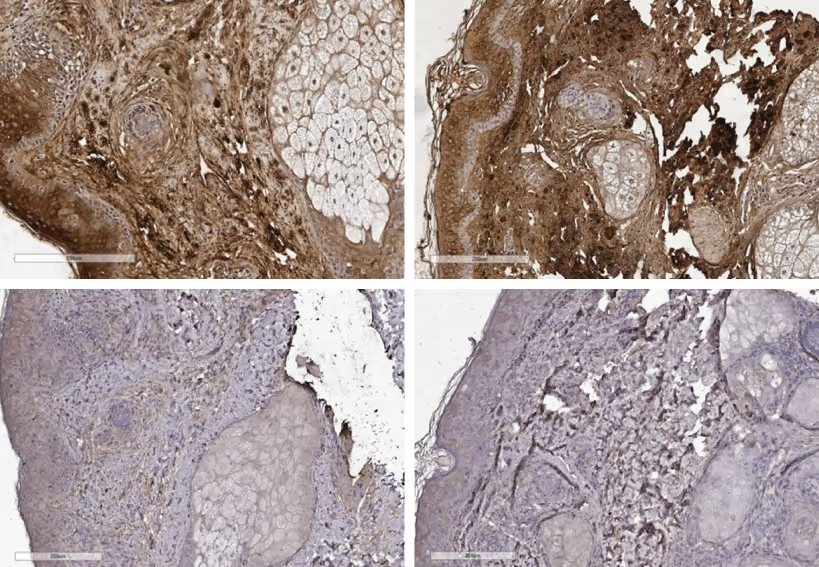
The mean expression area of type I collagen was 69.04 before treatment and 85.06 after, and of type III collagen was 1.81 before treatment and 3.06 after. When comparing of collagen type I and III expression areas before and after exposure, a statistically significant difference was found (p < 0.05).
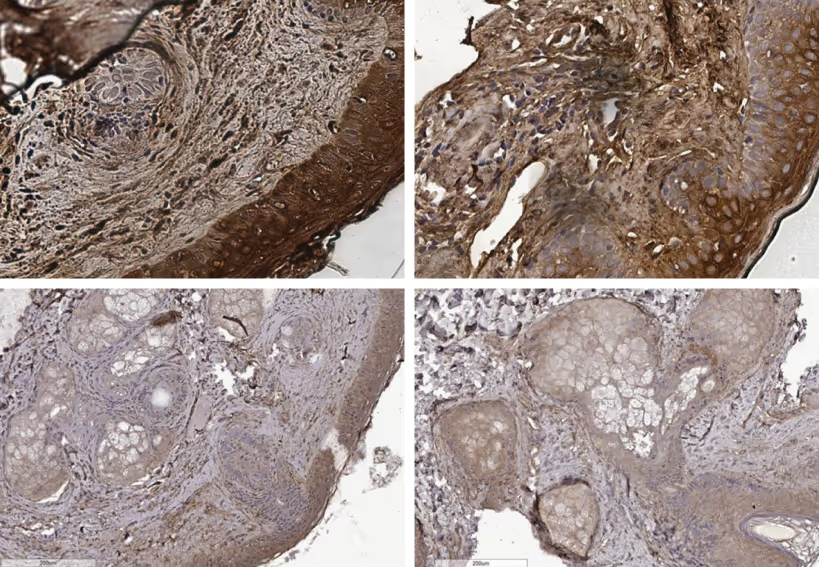
Patient Sh., 59 years old. The patient has normal skin type, prone to dryness, phototype II, even relief. Before treatment, the histologic preparation showed epidermis of typical structure, containing several hair follicles and a small number of sebaceous glands. The papillary and upper dermis was represented by loose connective tissue with a small number of vessels, the lumen was dilated, and a few vessels were gaping. The middle dermis contained large collagen and moderate lymphocytic infiltrate located in the circle of follicles. In B-G staining, the dermis was represented by thick, large fibers of connective tissue with a moderate amount of elastic fibers.
The dermis was characterized by immature collagen. After exposure, B-G staining in the upper and middle dermis showed alternation of large and small fibers with a significant number of elastic elements (Fig. 9).
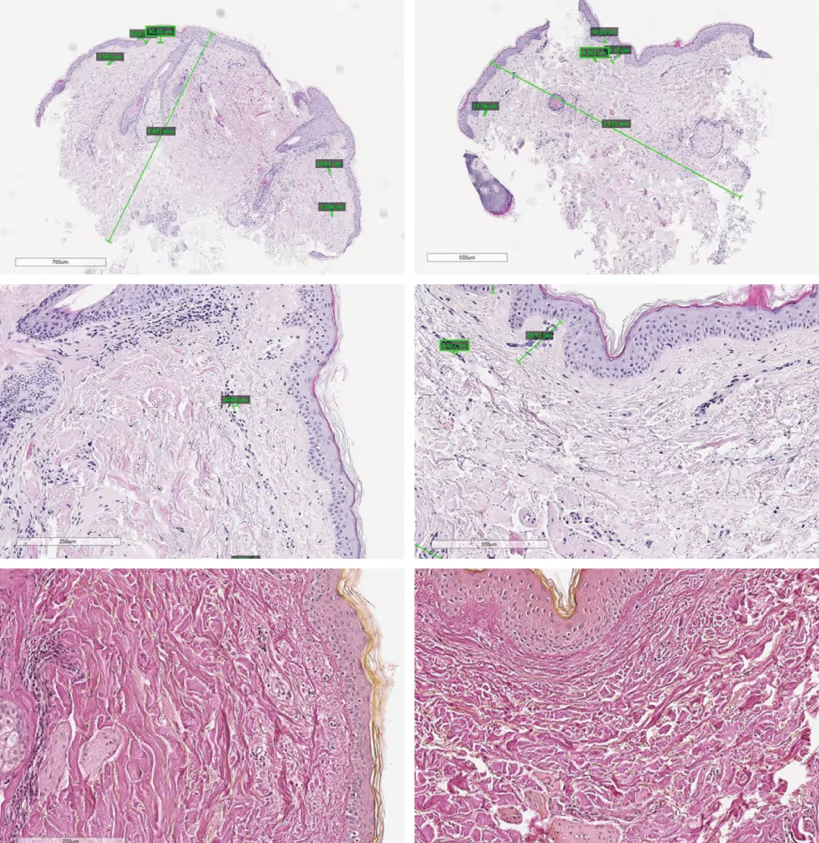
When comparing the samples, the disappearance of inflammation was noted, the dermis contained a large number of elastic fibers and collagen fibers of large and medium size, evenly distributed (Fig. 10).
The mean area of expression of type I collagen before treatment was 51.45, after - 68.7, type III collagen before treatment - 1.42, after - 3.43. Comparison of expression areas before and after exposure revealed statistically significant differences (p < 0.05) in the expression area of type I and type III collagen.
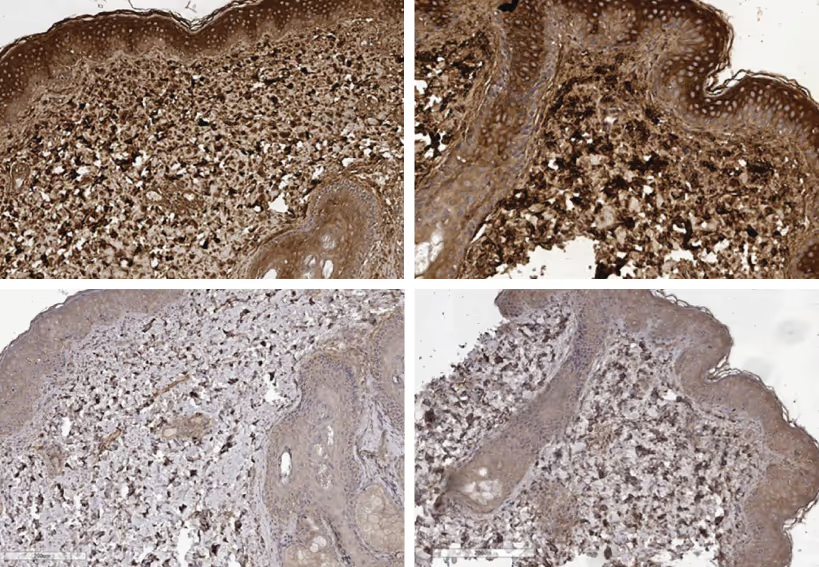
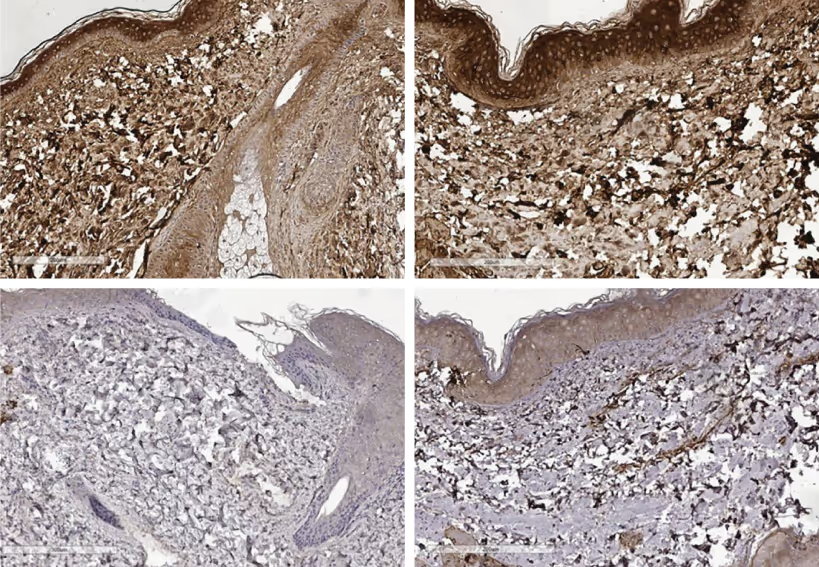
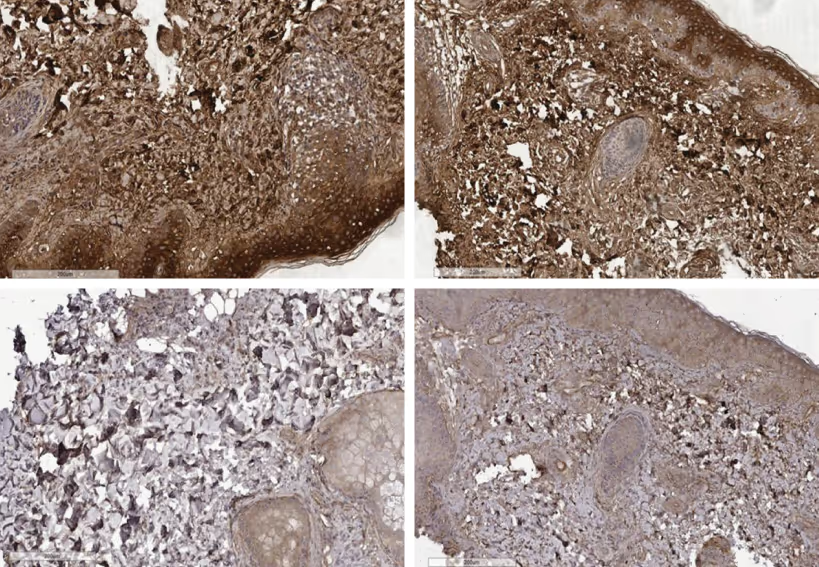
Patient A., 45 years old. The patient has an oily skin type, phototype II, even relief, marked diffuse and follicular hyperkeratosis.
Before treatment, the histologic preparation showed thin skin, epidermis of typical structure with keratinization. The papillary and upper dermis was represented by loose connective tissue with a small number of vessels, the lumen was closed, and some were gaping. The middle dermis was friable, contained hair follicles and sebaceous glands with signs of hypersecretion. In B-G staining, the dermis was represented by loose, thin fibers of connective tissue (pink) and elastic fibers (yellow). After laser exposure, mature collagen (red) forming thick bundles was detected in the papillary dermis in B-G staining (Fig. 11).
When comparing the samples, significant changes in lymphatic vessels with their dilation and appearance of lymphocytic infiltration, as well as enlargement of collagen fibers in the upper dermis were detected (Fig. 12).
The mean area of expression of type I collagen before treatment was 81.6, after - 82.63, type III collagen before treatment - 3.74, after - 9.23.
The comparison of expression areas before and after laser exposure revealed statistically significant differences (p < 0.05) in the expression area of type III collagen and no differences (p > 0.05) in the expression area of type I collagen.
Patient S., 47 years old. The patient has dry skin type, phototype II, even relief. Before treatment, the histological preparation showed epidermis with foci of hyperkeratosis, acanthosis foci, a small number of sebaceous and sebaceous glands. The upper dermis was friable, a small number of dilated vessels, lymphatic capillaries were narrow. The middle dermis was friable, containing a small number of large fibers.
In B-G staining, few large fibers with chaotic arrangement, a moderate amount of elastic fibers and thin collagen were visible. After exposure, large fibers alternated with elastic fibers and small collagen fibers in B-G staining (Fig. 13).
When comparing preparations before and after, changes in lymphatic capillaries with their sharp dilation were observed. The number of elastic fibers increased and large collagen bundles acquired a regular and uniform distribution (Figure 14). The average expression area of type I collagen before treatment was 70.06, after treatment 72.24; type III collagen before treatment - 5.50, after treatment - 11.15. The comparison of expression areas before and after laser exposure revealed statistically significant differences (p < 0.05) in the expression area of type III collagen and no differences (p > 0.05) in the expression area of type I collagen.
Conclusion
According to the results of the study, when comparing the expression areas of collagen type I, statistically significant results were obtained in four out of seven patients, when comparing the expression areas of collagen type III, statistically significant results were obtained in six out of seven patients. Thus, maximum changes in the expression of collagen types I and III were obtained in younger patients, which implies that laser skin rejuvenation procedures should be started at the age of 35 to prevent skin aging. However, even in the patient who did not have statistically significant results of changes in the expression areas of collagen types I and III, histological examination showed improvement of skin quality: expansion of lymphatic and arterial vessels, increase in collagen density in the area of the skin appendages in the upper dermis - enlargement of elastic fibers, more pronounced parallel arrangement of them.
The presented technique allows to achieve optical selectivity, low scattering of neodymium laser, reduction of pulse duration less than the time of thermal relaxation of vessels and skin melanin. The results of the histological study confirm the correctness of the choice of the optimal combination of pulse duration 0.65 ms and pulse repetition rate (up to 1.5 Hz), as well as exposure to energies sufficient to achieve coagulation of the chromophore, which contributes to the reduction of the rehabilitation period and demonstrates the safety and effectiveness of this technique. All the above-mentioned allows us to recommend the developed complex technique for application in patients of different ages with involutional changes of the face and neck.
References
- Kubanov A.A., Zhilova M.B., Kubanova A.A. Skin photoaging: mechanisms of development, features of clinical manifestations. Vestnik dermatologii i venerologii. 2014; 5: 53-59.
- Shah A.R., Kennedy P.M. The aging face. Med. Clin. North. Am. 2018; 102 (6): 1041-1054.
- Bonte F., Girard D., Archambault J.C., Desmouliere A.. Skin changes during aging. Subcell Biochem. 2019; 91: 249-280.
- Alexiades-Armenakas M.R., Dover J.S., Arndt K.A. The spectrum of laser skin resurfacing: nonablative, fractional, and ablative laser resurfacing. J. Am. Acad. Dermatol. 2008; 58: 719-737.
- Gold M.H.. Update on fractional laser technology. J. Clin. Aesthet. Dermatol. 2010; 3: 42-50.
- Robati R.M., Asadi E. Efficacy and safety of fractional CO2 laser versus fractional Er:YAG laser in the treatment of facial skin wrinkles. Lasers Med. Sci. 2017; 32: 283-289.
- Hong J.S., Park S.Y., Seo K.K., et al. Long pulsed 1064 nm Nd:YAG laser treatment for wrinkle reduction and skin laxity: evaluation of new parameters. Int. J. Dermatol. 2015; 54: e345-e350.
- Dayan S.H., Vartanian A.J., Menaker G., et al. Nonablative laser resurfacing using the longpulse (1064-nm) Nd:YAG laser. Arch. Facial. Plast. Surg. 2003; 5: 310-315.
- Glogau R.G., Matarasso S.L.. Chemical peels. Trichloroacetic acid and phenol. Dermatol. Clin. 1995; 13: 263-276.
- Carruthers A., Carruthers J. A validated facial grading scale: the future of facial ageing measurement tools? J. Cosmet. Laser. Ther. 2010; 12: 235-241.